Future Fit: 'We need permanent solutions, not sticking plasters'
We need "permanent solutions" – that is the message from the boss of Shropshire's two main hospitals who is leading the shake-up of health services in the region.
In an open letter to the Shropshire Star, Simon Wright, chief executive of Shrewsbury and Telford Hospital NHS Trust, has defended the plan to downgrade one of the county's existing A&E departments.
Shorter hospital stays and fewer complications are among the benefits of having one enhanced A&E department, he said.
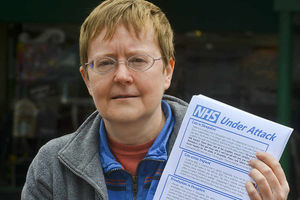
But in her open letter to the Shropshire Star, Gill George, from Shropshire Defend Our NHS, said downgrading an A&E department in Shropshire made "no sense" and has called for Future Fit to be scrapped.
It comes after the joint clinical commissioning group failed to reach a decision on whether to press ahead with the Future Fit review of healthcare.
The Future Fit review recommended that the best of four options would be to have one A&E serving Shropshire and Mid Wales at Royal Shrewsbury Hospital. The Princess Royal Hospital's Women and Children's unit would also be moved to RSH.
In his letter, Mr Wright said: "It's a fact that our acute emergency service has been frail for some time.
"We have recently secured two locum consultants in our A&E department. But the use of locums is not a long-term solution.
"We need permanent solutions, not sticking plasters.
"This isn't about 'downgrading' one of our hospitals. Under our plans, the hospital which does not have the emergency centre would host the majority of our planned care – the reason most of our patients come to hospital. This hospital would see and treat thousands of people every week.
"It is crucial that our population is able to engage formally in this process – and I look forward to the day when that begins."
But Ms George said: "No one has the faintest idea what happens next. Future Fit has run its course. It's time for health leaders to admit it's a complete shambles, and to walk away from it.
"Let's work together on an alternative where human beings come before budget cuts."
Open letters from Simon Wright and Gill George in full

There has been a great deal of comment across the media since last week's joint meeting of the two Clinical Commissioning Groups. Understandably, feelings are running high about this most important of issues.
Because this issue is so important, it's vital that we deal with facts and evidence rather than opinion and hearsay. It's a fact that our acute emergency service has been frail for some time. Just last winter, we met with health partners and patient representatives to discuss the best way of keeping patients safe in the event of these fragile services becoming unsustainable. These fragilities have not gone away.
We have recently secured two locum consultants in our accident and emergency department. But the use of locums is not a long-term solution. It is not sustainable to continue to pay the sums that locums command. Neither is the use of locums, who are not tied to the hospital and are free to move on at any time, good for continuity of care. We need permanent solutions, not sticking plasters.
Our plans to move to a single emergency centre, supported by two centres providing urgent care to the majority of people who currently attend A&E, would mean that our trust would become a more attractive place to work, increase emergency capacity and secure 24/7 senior review of all trauma patients, improving outcomes.
This is not just about the welfare of our staff; more importantly it is about the welfare of our patients. We cannot go on relying on the continued goodwill of clinical teams who are performing heroically every single day. Goodwill only goes so far and tired staff can sometimes make mistakes – this cannot be good for our patients, and we cannot continue like this.
Some argue: "How can closing an A&E be good for patient welfare?" I have said before and reiterate now that these plans are not about reducing two services to one, but about increasing two services to three. Our plans are for one emergency centre, treating the most seriously ill and injured patients; patients who cannot make their own way to hospital but will, in the vast majority of cases, arrive by ambulance.
The proposals will not see a decrease in the number of areas we have to treat urgent and emergency cases. We currently have a total of 43 clinical spaces. If our plans go ahead we would have 65 spaces, which is a 50 per cent increase in capacity.
Many of the conditions which we currently see in our A&Es would be treated at the centres for urgent care, which would be at both hospitals; most patients needing urgent attention will see no difference in the way they are treated.
This isn't about "downgrading" one of our hospitals. Under our plans, the hospital which does not have the emergency centre would host the majority of our planned care – the reason most of our patients come to hospital. This hospital would see and treat thousands of people every week.
Last year, we cancelled more than 370 planned hospital operations in our theatres due to last-minute emergency demand. Having a hospital which deals with the majority of our planned care would mean patients who attend our hospitals for planned operations wouldn't have their care affected by the need to prioritise seriously ill or injured emergency patients.
An elective centre would also be infection free, due to the separation of emergency care, leading to shorter hospital stays, fewer complications and better outcomes.
It is no secret that health budgets – nationally and locally – are stretched. And yes, these plans will bring savings which will help to address those challenges – but not at the cost of patient care. By configuring our hospitals in this way, we will, as I have said, become a more attractive place to work. This will reduce our reliance on agency and locum staff, who attract premium rates of pay.
Paying staff who are not members of SaTH more money than permanent members of staff though agencies is unfair and costs the trust millions of pounds every year. Duplicating emergency cover, loss of economies of scale and too few doctors to speed up treatment decisions all means longer stays in hospital and delays. This collective of costs is what we will save and invest back into our wider system.
Our planned clinical model has been drawn up by working doctors, nurses and other health professionals – those who are at the forefront of patient care today. They believe it provides the best solution for patients not just in the immediate future, but for future generations. However, it is vital that the people we serve are given the chance to look at the plans in detail, rather than relying on hearsay and rumour. It is crucial that our population is able to engage formally in this process – and I look forward to the day when that begins.
Simon Wright, chief executive of Shrewsbury and Telford Hospital NHS Trust
Three years of work, three years of broken promises, and about £3 million of NHS money down the drain.
And last week, Shropshire Clinical Commissioning Group voted to go forward, while Telford and Wrekin voted to press the pause button.
And no-one has the faintest idea what happens next. It's not impressive. Future Fit has run its course. It's time for health leaders to admit it's a complete shambles, and to walk away from it.
Future Fit is always posed in terms of "no change" versus "closing an A&E". They tell us "No change is not an option".
There's always scope for change, when change makes NHS services better.
I know that from working most of my adult life as an NHS clinician. It doesn't follow that any change is good. You have to start from the care patients need, and then look at how the NHS can deliver that.
We have a huge geographical area, Shropshire, Telford and Wrekin, and Powys. For people in rural areas, access to healthcare really matters: healthcare where people can get to it. It makes no sense to close an A&E and downgrade one of our hospitals, or to reduce our access to routine planned care (as Future Fit will also do). It makes no sense either to close or downgrade our rural services – but our rural maternity units are now under threat.
Future Fit will not solve the problems in our local A&Es. Our A&Es get full because there aren't enough hospital beds for patients needing to be admitted.
The hospital beds are full because there aren't enough community services – so patients can't be discharged.
And because the A&Es get full, ambulances stack up outside, and can't respond to 999 calls. The whole system seizes up.
This is what needs sorting out in our local hospitals – yet they plan to move to a single A&E with a capacity less than half of our existing A&Es! That's no solution.
Making patients travel long distances to A&E won't matter for some patients, but for others, longer journeys will result in worse outcomes or even death.
Yes, there are problems recruiting emergency consultants locally – just like 80 per cent of hospitals in the UK.
Local problems are over-stated though. Our hospital trust has just recruited two locum emergency consultants, with no great difficulty. They won't go permanent because their pay would be cut. As the Royal College of Emergency Medicine says: better pay and conditions would solve the problems. And when local hospital bosses stop saying they're about to close the A&E, they might find it's easier to recruit.
There are other problems. Future Fit is part of a bigger cuts package, the Sustainability and Transformation Plan. They plan to cut a shocking 2,000 jobs in our local NHS. What will that mean for services – and for the sacked staff? Local NHS spending will be cut by £150 million a year. There are already plans for a £3.8 million cut to community hospitals and community hospital beds, with millions more saved by rationing hip and knee replacements. They expect volunteers to fill the gaps, but it's not realistic. Friends and neighbours can't just take on the work of doctors, nurses, therapists and carers.
There's a big question here. What kind of society do we want to live in? The UK spends way less on health than other developed countries, and we're dropping further and further behind. This is why our NHS in Shropshire is starting to fail. If our choice is to live in a community that cares for our sick, elderly and vulnerable members, then it's time to stop the cuts in health and social care.
And Future Fit? It's Future UN-Fit, no longer fit for purpose. Let's work together on an alternative where human beings come before budget cuts.
Gill George is chair of Shropshire, Telford and Wrekin Defend Our NHS





