Shropshire hospitals have improved but must do more, says CQC
Two-thirds of the areas inspected were rated as good, but long A&E waiting times and a reliance on agency staff were criticised.

Improvements are still needed at Shropshire’s two main hospitals, a new inspection report has revealed today.
A report by the Care Quality Commission (CQC) said the trust which controls Royal Shrewsbury Hospital and Telford’s Princess Royal has made improvements and is effective and caring. A total of 64 per cent of the areas inspected were rated as ‘good’.
But long waiting times in A&E, a heavy reliance on agency staff and a lack of consultants and middle-grade doctors contributed to the trust being given an overall ‘requires improvement’ rating.
Warnings were issued when the hospitals were last inspected in 2014 and also given a ‘requires improvement’ rating.
At the time inspectors had particular concerns about end of life care at RSH, which was rated inadequate.
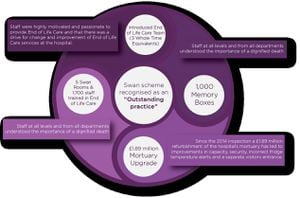
Since the last inspection, inspectors said they could see that the trust had made significant improvements in a number of areas, including end of life care, surgery and medical care. They also noted a positive change in culture amongst staff and leaders.
The trust’s rating for providing effective services had also improved and was upgraded from ‘requires improvement’ to ‘good’.
Simon Wright, chief executive of the trust, said while there was “still more to do” the trust was in “a much stronger position than two years ago”.
He said a lot of work had already been done since the inspection, and he was inviting the CQC to return to see the improvements.
The inspection found the trust’s two emergency departments were experiencing continued pressure and a shortage of consultants and middle grade doctors meant that some patients had to wait too long for an initial clinical assessment.
The findings, following inspections in December and January, found the process for patients brought in by ambulance was inconsistent and unstructured and nursing staff vacancies were impacting on continuity of care.
The report said: “Two consultants told us they were supposed to attend between 9am and noon on weekends, to carry out ward rounds in ED and the clinical decisions unit. However, they said they rarely left the department before 5pm and were then frequently called back in overnight. They told us this level of pressure was unsustainable.”
In maternity services inspectors found that safety needed further improvement. Inspectors said a lack of regular postnatal ward rounds meant high risk postnatal women were not regularly reviewed and on the Wrekin Midwife Led Unit medicines management was also a concern.
However, there were areas of ‘outstanding practice’ which inspectors highlighted including the trust’s Swan Scheme for bereaved families and the trust’s partnership with The Virginia Mason Institute in the US– regarded as one of the safest hospitals in the world.

Inspectors praised staff and said in every interaction they saw between nurses, doctors and patients, the patients were treated with dignity and respect.
They said staff were highly motivated and passionate about the care they delivered.
The report stated: “We saw examples of good care being given on every ward and department we visited.”
The CQC has said the trust must make a number of improvements:
All patients brought in by ambulance must be promptly assessed and triaged by a registered nurse.
The trust must ensure its emergency department meets the Department of Health’s target of discharging, admitting or transferring 95 per cent of patients within four hours of arrival in the department.
Sufficient nursing staff must be on duty to provide safe care for patients.
A patient acuity tool should be used to assess the staffing numbers required for the dependency of the patients.
Medical staffing must be reviewed to ensure sufficient cover is provided to keep patients safe at all times.
All staff must have up to date mandatory training.
The trust must ensure it meets the referral to treatment time for admitted pathways for surgery.
Staff must have an understanding of how to assess mental capacity under the Mental Capacity Act 2005 and assessments must be completed.
The trust must ensure the application of the World Health Organisation’s (WHO) ‘five steps to safer surgery’ checklist is improved in theatres.
The prevention, detection and control of the spread of infection, associated with the mortuary department, must be ensured through the decontamination of surgical instruments and making sure arrangements are in place for regular deep cleaning.
The report’s main positives points
Openness and transparency about safety was encouraged. Incident reporting was embedded among all staff, and feedback was given.
In every interaction inspectors saw between nurses, doctors and patients, the patients were treated with dignity and respect.
Staff were highly motivated and passionate.
Treatment was planned and delivered in line with national guidelines and best practice recommendations.
Local and national audits of clinical outcomes were undertaken and quality improvements projects were implemented in order to continually improve patient care and outcomes.
It was easy for people to complain or raise a concern and they were treated compassionately when they did so.
There was a clear statement of vision and values, driven by quality and safety. Leaders at every level prioritised safe, high quality, compassionate care.
The trust had made end of life care one of its priorities in 2015/2016.
Staff were encouraged to report incidents and felt able to do so
There were effective systems and processes to ensure that vulnerable adults and children were safeguarded.
Outcomes for people who use service were generally positive and mostly met expectations.
The NHS Friends and Family Test (FFT) survey results were better than England averages.
The primary negative points in the report
The trust’s referral to treatment time for admitted pathways for surgery have been lower than the England overall performance since September 2015.
There were insufficient numbers of emergency department consultants for the size of the department, consultants work excessive hours
The trust was below the national average for junior medical staff
There was a heavy reliance on agency and locum staff to ensure that shifts were filled
Thermometer information was not displayed on wards.
The maternity specific safety thermometer was not being used to measure compliance with safe quality care.
Mortuary staff decontaminated surgical instruments manually at PRH; this exposed staff to unnecessary risk and did not provide a high level of disinfection.
Nursing staff vacancies were impacting on continuity of care and an acuity tool was not used to assess staffing requirements.
Inconsistencies were identified in the staffs application of the World Health Organisation’s (WHO) ‘five steps to safer surgery’ checklist.
In maternity services, feedback to staff on incidents was described as inconsistent and only a few midwives told inspectors they had received feedback.
The trust was not achieving the Department of Health’s target to admit, transfer or discharge 95 per cent of patients within four hours of their arrival in ED.
Compliance with the trust target for completion of staff appraisals was below the trust target.